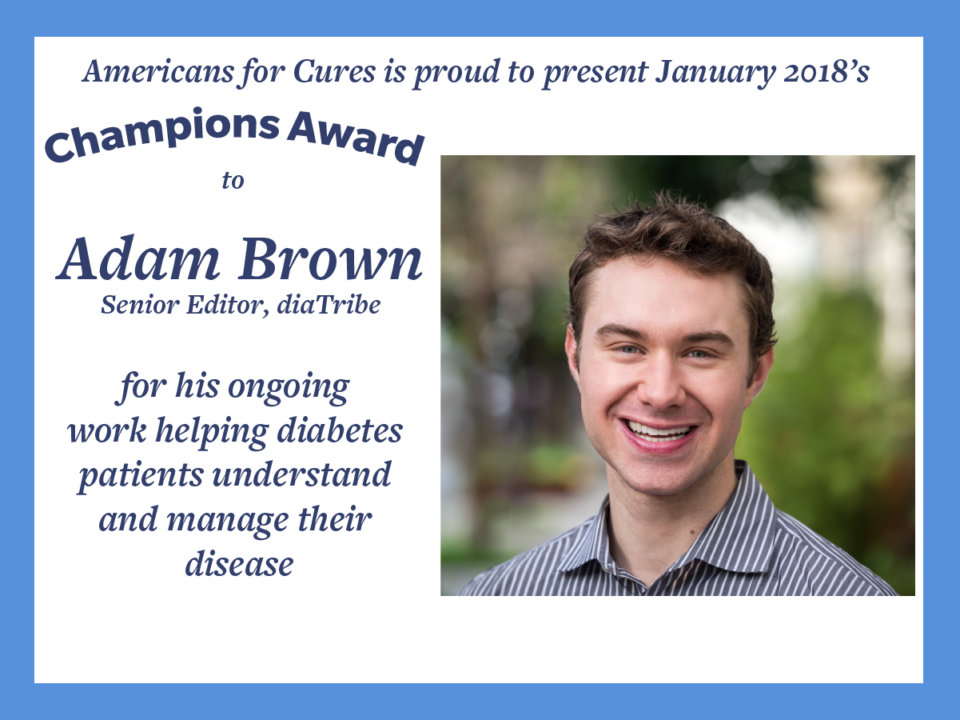
Meet January’s Champion Award recipient, Adam Brown. He was diagnosed with diabetes in 2001 at the age of 12. He now writes and speaks extensively about diabetes and chronic disease, and is recognized as a leading expert in diabetes technology. Today, Adam is a Senior Editor at diaTribe—a nonprofit devoted to helping diabetes patients better understand their disease and stay healthy—where he writes a weekly column. He also leads Diabetes Technology & Digital Health at Close Concerns.
We spoke with Adam to learn more about his experience of living with diabetes and what motivates him to do the important work of helping patients understand their disease.
Q: What’s your story of being diagnosed with diabetes?
I was diagnosed with diabetes at 12 years old with the textbook symptoms: fatigue, urinating all the time, constantly thirsty, and losing weight. I remember feeling shocked and crying at the news – “You have diabetes” – and most of that time is a blur. But I do remember struggling mightily, and I certainly recall feeling like a failure at every doctor’s appointment.
I’m the oldest of six kids, which pushed me to quickly take ownership of my own diabetes from a very young age. But the diabetes tools were not as good back then, and the instructions on what to do were poor. I checked my blood glucose (“BG”) around four times per day, rarely finding myself in an ideal range. My A1c was far too high at 8%-9%, and the daily swings from 45 mg/dl to 300 mg/dl put me at high risk of seizures from extreme low BGs (hypoglycemia) and long-term damage from extreme high BGs (hyperglycemia). It took many years before I found my way, a path I’ve tried to summarize in Bright Spots & Landmines.
Q: Did you have any misconceptions about diabetes before your diagnosis that you didn’t realize until after?
I honestly didn’t know much about it. In 2001, diabetes was rarely talked about, and I certainly didn’t learn anything about it in school.
Q: What were the most surprising changes to your lifestyle after you were diagnosed?
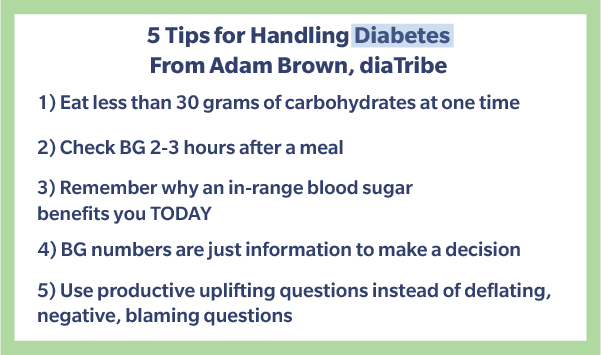
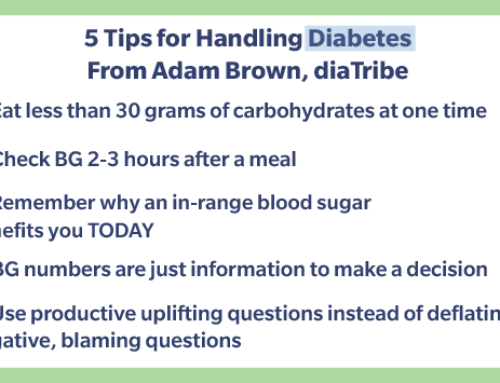
This is the crux of why I struggled so mightily – we didn’t make major food changes! The terrible advice we got at diagnosis was, “You can eat what you want, as long as you take insulin for it.” What absurd advice to give to anyone with diabetes, especially a teenager! This was a blank check not to change my diet at all, so I didn’t: sleeves of crackers, triple cheeseburgers with fries, stacks of cookies, plates of pasta the size of my head – you get the idea. As my mom told me recently, “We were a carb-centric family and always had a treat after supper!” Dosing insulin for high-carb, high glycemic foods is insanely difficult – even with the continuous glucose monitoring (CGM) devices we have in 2017 – let alone on the four fingerstick data points I was using back then.
I remained just as active, playing three sports in grade school, but you cannot out-exercise a bad diet.

Adam Brown, center, with his five siblings.
Q: We’ve read that people with diabetes have to make up to 300 decisions daily to manage their disease. Describe how diabetes affects your day-to-day choices.
Diabetes can invade every area of life – thoughts, energy levels, relationships, ability to do things that make me happy, etc. When my blood sugars are in range, I’m my “best self.” But there are more than 22 factors that influence blood sugar, which brings up a multivariable calculus problem many times per day.
Every time I eat, for instance, I’m assessing what my blood sugar is, where it’s trending, the balance of fat/protein/carbs, the amount of food on the plate, how much insulin I should take, what patterns I’ve seen today and recently, what happened the last time I ate this, whether I’m going to go for a walk after dinner, and beyond. All the human cognitive biases play a role, and the math problems don’t end at meals – exercise, sleep, travel, stress, device malfunctions, and more all influence blood sugars in any given moment. These variables all interact in complicated ways, which means even the best-informed decisions don’t pan out into in-range blood sugars.
This is one of the reasons I wrote Bright Spots & Landmines – I wanted a single guide to summarize all the most effective decisions that: (i) work consistently; (ii) help me minimize mistakes; and (iii) reduce the decision-making burden.
Q: You write a bi-weekly column for diaTribe called Adam’s Corner. How did you first get involved with diaTribe?
I began working at diaTribe as part of my summer internship in 2010. I absolutely loved it, and when the summer was over, I accepted an offer to return full time after college. Back then, diaTribe was once-monthly, and we mostly focused on research and product news. After a couple years, I thought it might be cool to write a personal column in diaTribe. My goal was to be highly actionable and provide tips for navigating food, mindset, exercise, and sleep.
Writing for diaTribe has been one of the greatest experiences – and biggest honors – of my life. I feel so energized every time we get a reader email and hear that our writing has helped someone.
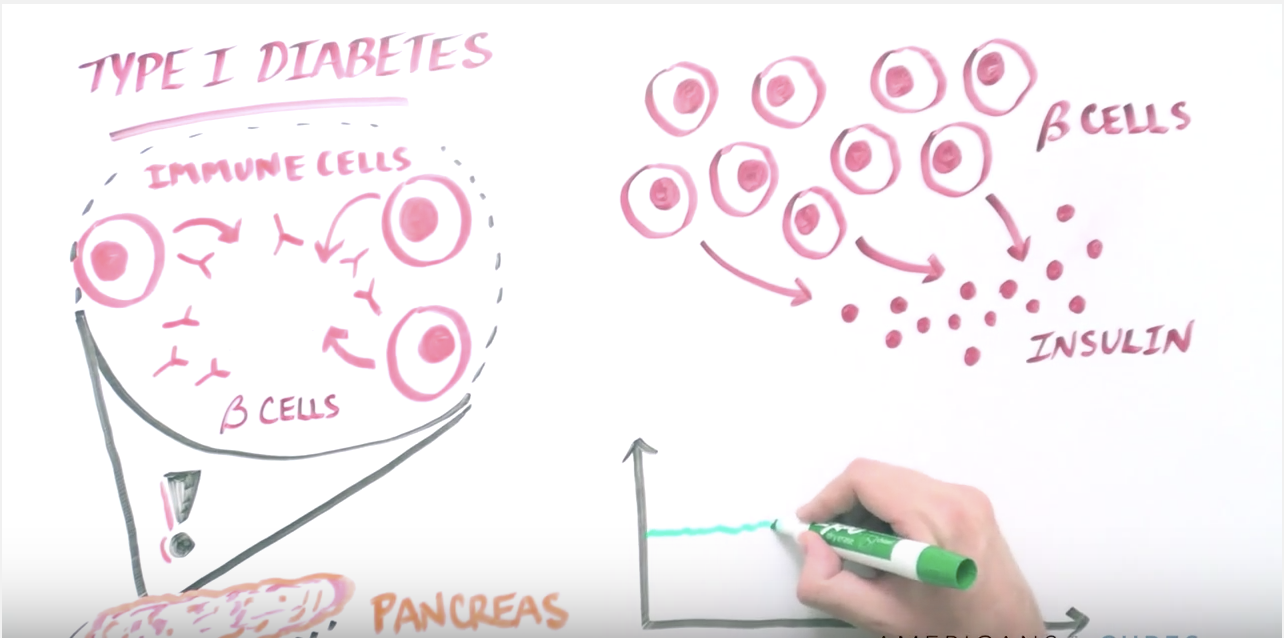
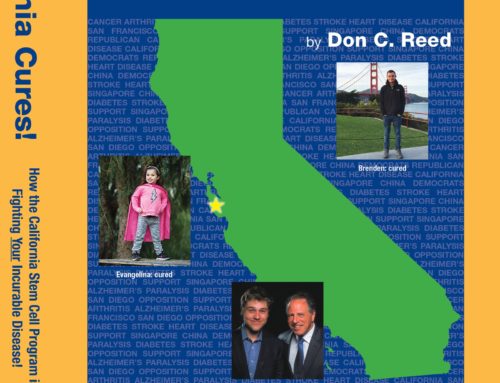
Q: How has stem cell research altered the conversation for diabetes patients?
Stem cell research is an exciting area of long-term research as we talk about “curing” diabetes, however far away that is. If we can take stem cells, differentiate them into beta cells that produce insulin, and successfully protect them from the immune system, it would be a tremendous step forward for type 1 diabetes.
Beyond his writing, Adam has shared his patient perspective at numerous venues since 2010, including local and international conferences, FDA and NIH meetings, and the field’s largest scientific gatherings. He graduated summa cum laude from the Wharton School of the University of Pennsylvania in 2011 as a Joseph Wharton and Benjamin Franklin Scholar. Adam spends his free time outside in San Francisco drinking tea, hiking with his girlfriend Priscilla, and teaching his old dog new tricks. You can get his book, Bright Spots & Landmines, here.