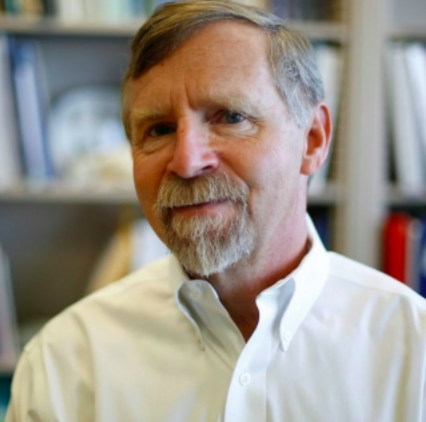
Meet Dr. Dennis O. Clegg. He is professor and principal investigator at the University of California, Santa Barbara’s (UCSB) Clegg Lab. Dr. Clegg’s research focuses on neural development and regeneration with studies of extracellular matrix and integrin function in the developing eye. His current emphasis is in stem cell research, with a focus on developing therapies for ocular disease. He is founder and Co-Director of the UCSB Center for Stem Cell Biology and Engineering, and has served on advisory boards for the California Institute for Regenerative Medicine and the National Institutes of Health Center for Regenerative Medicine.
We spoke to Dr. Clegg about his research and how stem cells are being used to treat diseases that affect vision.
Q. What is one new and exciting stem cell discovery in your area of research?
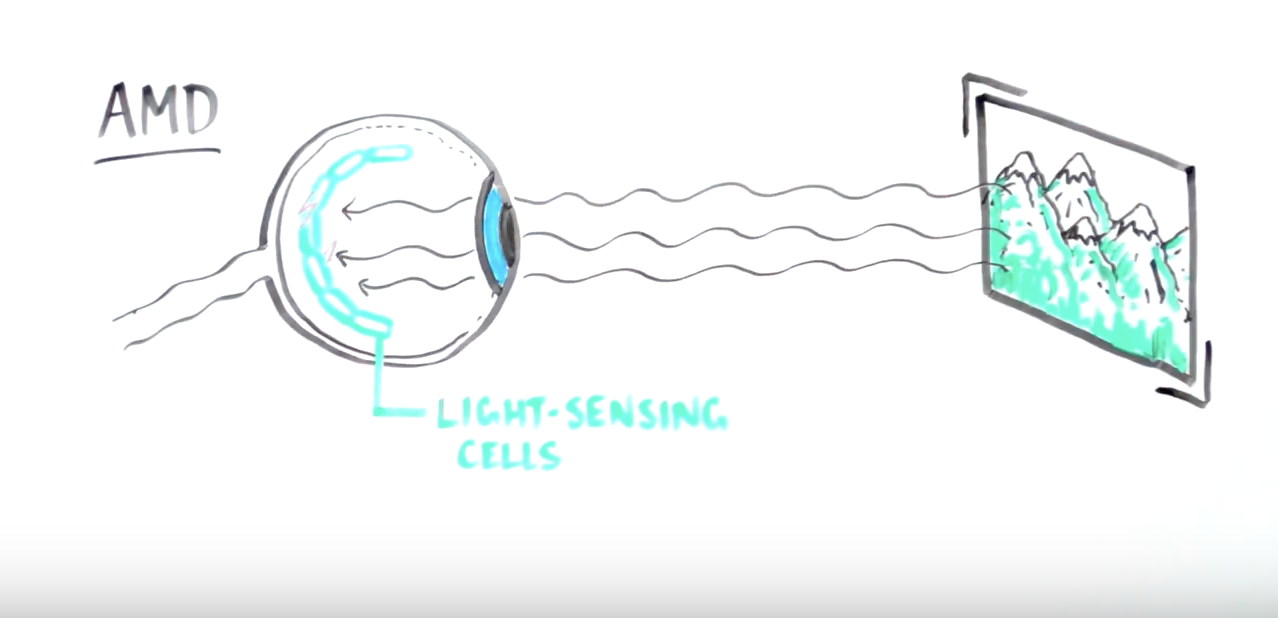
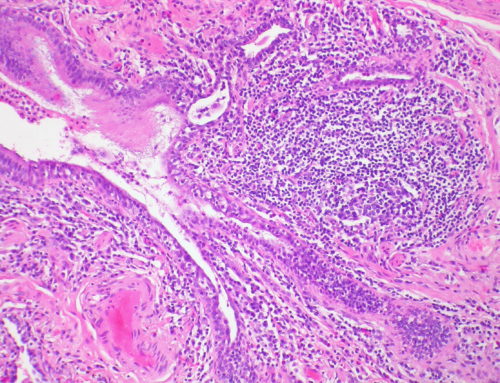
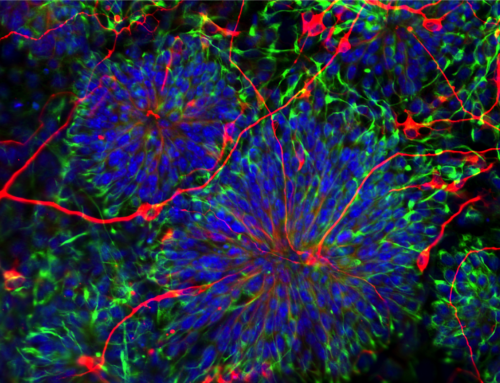
My area is cell therapy for the dry form of macular degeneration (AMD). There are two forms of AMD: for the wet form, there are existing treatments but the dry form has no effective therapy yet. Vitamins are often used but those only slow the progression of the disease. The disease is caused by loss of retinal pigment epithelium (RPE) cells that are in the back of the eye and are support cells for the rods and cones (photoreceptors). These photoreceptors enable us to see. And when the RPE dies, so do the photoreceptors.
Our idea: Go in early with our stem cells, replace the RPE, and keep the photoreceptros happy! We grow the RPE cells on scaffolds (like contact lenses). And the surgeons implant these in the back of the eye.
In collaboration with USC, Cal Tech, City of Hope, and Regenerative Patch Technologies , we are now running a Phase I/IIa clinical trial at USC using this therapy.
We are hopeful about the results of our first cohort of patients. Sadly, others recently did a clinical trial using a molecule that was a complement inhibitor and it did not work. So we are all looking for other ways to treat AMD. I’m super enthusiastic about cell therapy for this disease. Most importantly, the patients who are enrolling in these clinical trials are like astronauts going into space. We tell them this has never been done before but they are open to trying. They are my heroes.
Most importantly, the patients who are enrolling in these clinical trials are like astronauts going into space. We tell them this has never been done before but they are open to trying. They are my heroes.
I’ve been working on retinal development and retinal disease for a very long time. So it’s rewarding to see this progress from bench to bedside.
Q.What is the best way for advocates to rally support for stem cell research?
We are in touch with the local braille society. We’ve done outreach to low vision clinics where ophthalmologists, optometrists, and families all join together, not just for AMD but also for Retinitis Pigmentosa (RP) – another form of vision loss. These groups have been very supportive and they even organize a golf tournament for fundraising for research towards treatments but also for raising awareness. Even the young generations get involved. We have a young lady who has early onset AMD and is a girl scout. For her eagle scout, she is fundraising for research…she’s thinking big! So, there are many different ways to advocate for stem cell research.
Q. You’re at a dinner party and someone asks you why you believe in the power of stem cells to treat chronic conditions. What is your response?
They have tremendous potential for treating a number of different diseases. When embryonic stem cells were first derived from humans in 1998, it caught my attention and I saw a lot of potential. There are so many untreated diseases now. So, if there is a path towards helping patients, it’s worth working on.
Another thing I tell people at dinner parties though is: Use authentic stem cells. Don’t go to unproven “stem cell clinics”. There are now so many of them and it’s important to be cautious and look for evidence-based therapies and trials.