About
Diabetes can be divided into two main types — Type 1 and Type 2:
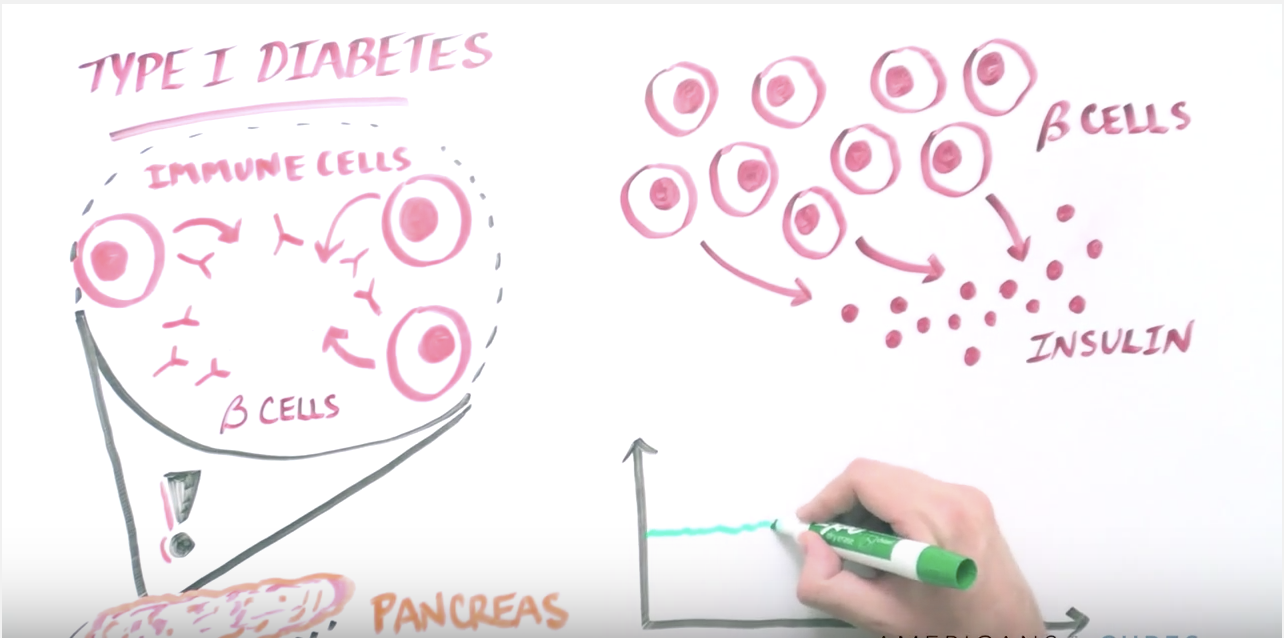
- Type 1 Diabetes (T1D): An autoimmune disease where the insulin-producing beta cells in the pancreas are destroyed by the body’s own immune system. T1D has a genetic component that can be diagnosed both early in life and in adulthood. There is currently no cure for T1D, but patients rely on injected or pumped insulin to survive. Without insulin, the cells starve, and sugar builds up in the bloodstream, causing damage to the kidneys, blood vessels and retina.
- Type 2 Diabetes (T2D): A metabolic disorder often diagnosed later in life and can be due to either genetic predisposition and/or lifestyle habits. T2D patients can produce insulin, but their bodies are unable to use it effectively. T2D can be typically managed with diet and exercise or medication, but more serious cases may require insulin therapy.
How Stem Cells Can be Used to Treat Type 1 Diabetes
- Stem cells can either replace the lost beta cells or protect the existing cells from dying.
- Alternatively, stem cells could serve as a source for insulin production.
- Lastly, stem cells could modulate the immune system and decrease immune attack of pancreatic cells.
CIRM’s Progress: Selected Research Highlights
- CIRM has funded four clinical trials for T1D across three California institutions. Some examples, include:
- In a Phase 1/2 clinical trial, UCSF researchers are studying how co-transplantation of islet cells (which are dying in T1D) and parathyroid glands (which are responsible for immune regulation) from the same donor can aid in the transplantation success.
- In a Phase 2 clinical trial, Caladrius Biosciences is modifying the patient’s own immune system to reduce autoimmune attack.
- In two Phase 1/2 clinical trials, ViaCyte is developing different techniques to “shield” stem cells before delivery into T1D patients where the transplanted cells will not be prone to autoimmune attack and can produce insulin. These studies have demonstrated promising results of engraftment and insulin production.
- CIRM has also funded numerous early stage and pre-clinical studies in this area. Some examples include:
- CIRM-funded researchers have developed methods of creating replacement insulin-producing cells from stem cell lines that can be grown in large numbers. These cells could then be delivered inside a device that would protect the cells from the immune system. .
- Other CIRM-funded research is studying how to regulate the immune system in order to make stem cell-derived transplants safer.
- Late-stage research from UCLA aims to bring methods of genetically matching donor and host cells so that pancreatic stem cells can be delivered to T1D patients without the need for aggressive immunosuppression.
Diabetes Organizations Organizations Endorsing YES on Prop 14
To see the full list of over 80 patient advocate organizations that endorse YES on Prop 14
please click hereTYPE 1 DIABETES
Type 1 Diabetes (T1D) develops when a person’s own immune system mistakenly destroys the insulin-producing cells in the pancreas, called “beta cells.” Blood sugar levels can spike when this happens, causing organ and nerve damage, heart disease, limb amputation, or even death.