About
- In 2018, California was the state with the highest number of new HIV diagnoses.
- California accounts for about 12% of all HIV/AIDS cases in the U.S. with over 135,000 Californians living with HIV/AIDS in 2017.
- The direct healthcare cost of HIV/AIDS to the state, not including the personal, social and work productivity losses, is projected to be nearly $1.8 billion per year. For every 100 people with HIV in 2018, only 56 were virally suppressed, and only 65 received some HIV care.
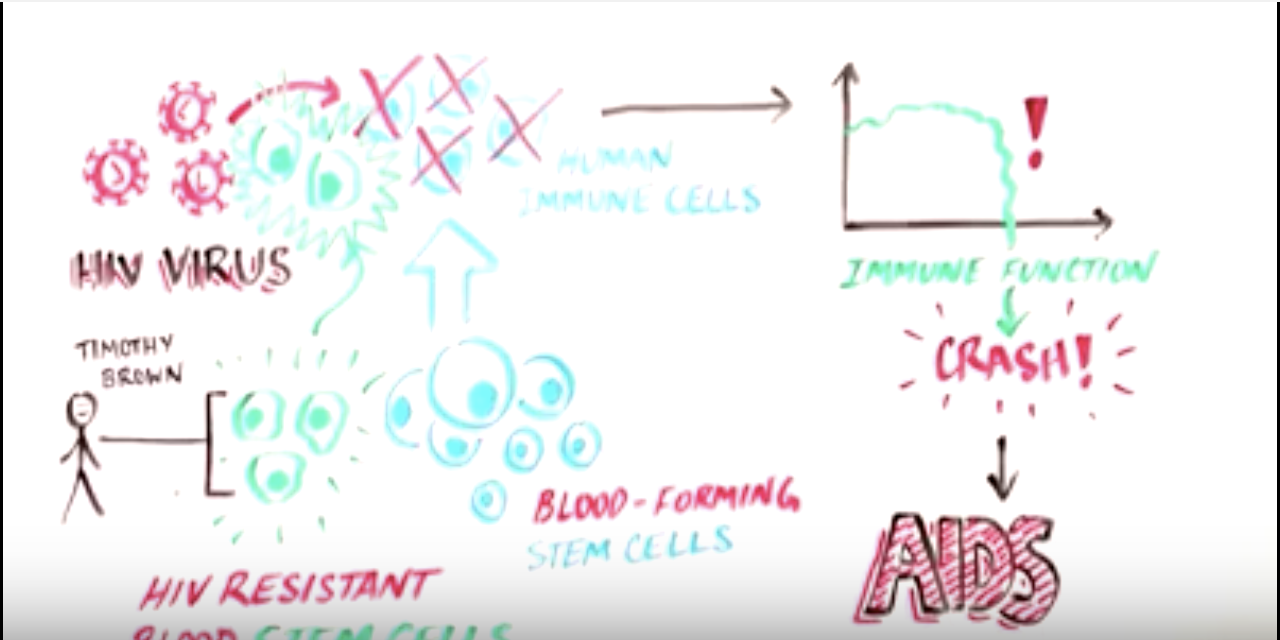
- The human body cannot eliminate HIV and there is currently no effective HIV cure. This means that once a person has HIV, they have it for life. Anti-retroviral medication is available, but is not curative — it must be taken daily for the rest of a patient’s life.
- If left untreated, HIV can lead to the disease AIDS (Acquired ImmunoDeficiency Syndrome).
- AIDS is the late stage of HIV infection that is the result of immense damage to the body’s immune system. Most HIV positive people in the U.S. do not progress to AIDS because daily HIV medication is prescribed, stopping the progression of the disease and preventing its spread. Without HIV medication, people who develop AIDS typically only survive for an average of 3 years.
How Stem Cell Research Can be Used to Treat HIV/AIDS
- One of the key stem cell approaches to treat HIV/AIDS involves replacing an infected person’s immune system with one that the virus cannot infect. Specifically, the CCR5 gene makes a protein that is required for HIV to enter cells. A mutation in the CCR5 gene that naturally occurs in some people has been identified to be protective against HIV, and an effective bone marrow transplant from a person with this genetic mutation can (and has) effectively cured a person with HIV.
- However, because there are not enough people with this naturally occurring CCR5 genetic mutation to provide bone marrow transplants for all HIV patients, stem cell scientists are working on ways to create CCR5 mutations in the laboratory using HIV patients’ own blood-forming stem cells and mutating the CCR5 gene, which would then repopulate the person’s own blood system with one that lacks CCR5, disallowing the HIV virus to infect.
CIRM’s Progress: Selected Research Highlights
- CIRM has funded three clinical trials across three California institutions. Some examples include:
- In a Phase 1 clinical trial, City of Hope researchers are studying ways to mutate the CCR5gene using a novel tool that acts as a pair of molecular scissors, snipping the CCR5 gene at the exact spot that disallows HIV to infect.
- In a Phase 1/2 clinical trial, UC Davis researchers are studying how a patient’s blood-forming stem cells with 3 anti-HIV genes inserted into them create HIV-resistance in individuals to prevent the return of AIDS-related lymphoma.
- Researchers at UCLA are studying methods of engineering life-long cellular immunity to HIV. This research seeks to genetically modify blood-forming stem cells so that they can identify and eliminate the HIV.
HIV/AIDS Organizations Endorsing YES on Prop 14
San Francisco AIDS Foundation