There are three types of stem cells: adult stem cells, embryonic (or pluripotent) stem cells, and induced pluripotent stem cells (iPSCs).
Adult/Tissue Stem Cells
Adult stem cells, or “tissue stem cells,” can come from different parts of the adult body. They are specific to a certain kind of tissue in the body: for instance, liver stem cells can regenerate liver tissue, and muscle stem cells can regenerate muscle fibers. But adult stem cells are limited to only becoming more of their specialized tissue—liver stem cells cannot make new muscle fibers, nor can muscle stem cells make new liver tissue.
Embryonic/Pluripotent Stem Cells
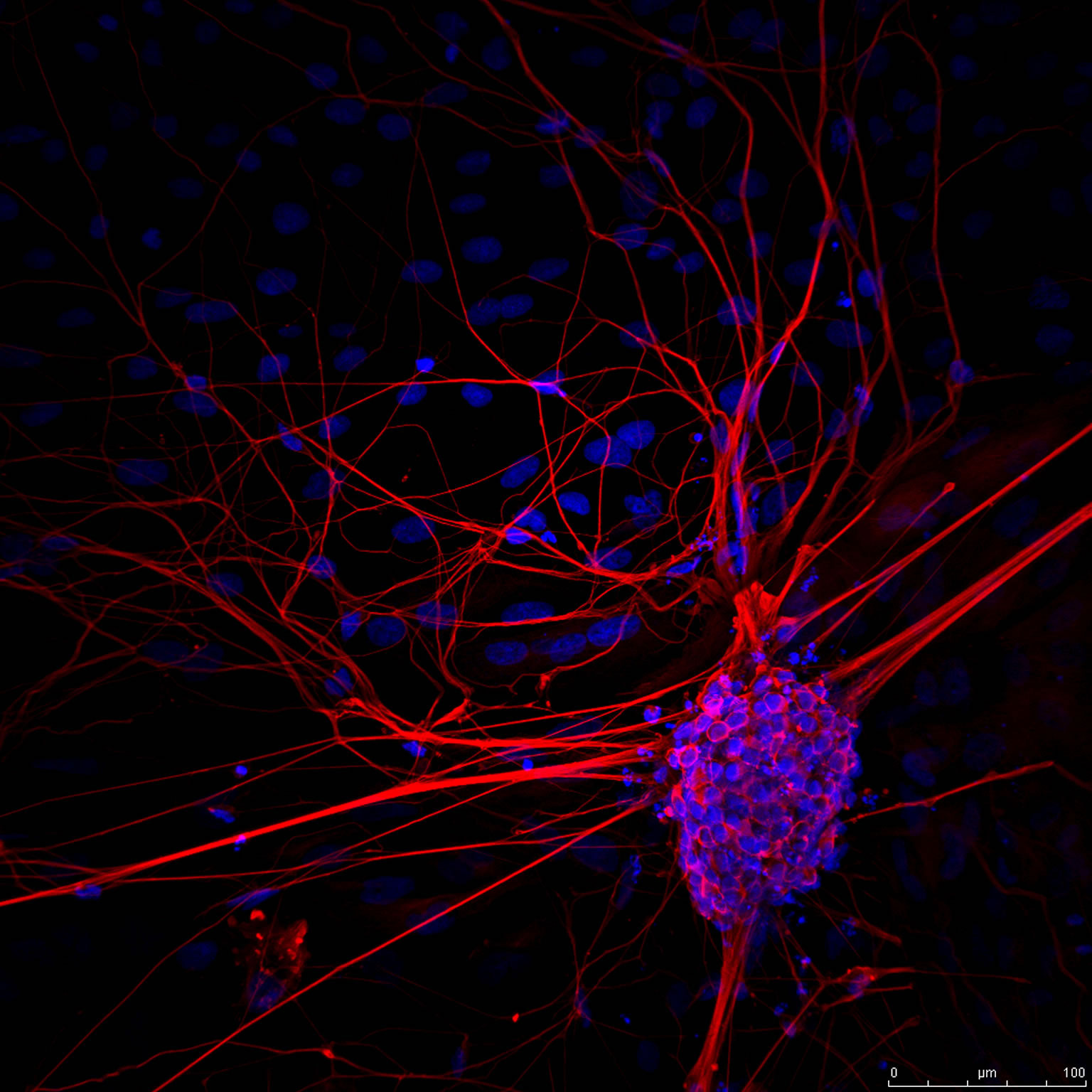
The thousands of different cell types that make up our bodies all came from one single “master builder” cell, called a pluripotent stem cell.
Pluripotent stem cells can be thought of as “blank slates,” because of their ability to build any cell type in the body—skin cells, brain cells, muscle cells, etc. Unlike tissue stem cells, pluripotent stem cells are not limited to only becoming more of a certain tissue.
Pluripotent stem cells primarily consist of embryonic stem cells, but the term now also encompasses another type of cells, called “induced pluripotent stem cells.” More on that later.
Induced Pluripotent Stem Cells/iPSCs
Induced pluripotent stem (iPS) cells are pluripotent cells that are derived from adult tissue using new scientific technology. They share characteristics with embryonic stem cells in that they can become any cell type in the body.
Reprogramming stem cells to create iPSCs involves some genetic manipulation, and this may cause some differences that are not present in cells that are already embryonic in nature. It is essential to continue research using all cell types. Because the field of stem cell research is so new, it is critical to explore all avenues of stem cell research, from pluripotent to tissue stem cells.
The process of generating an iPS cell line takes time and resources in a lab. To do so in a sterile and safe way in which the cells can be transplanted back into someone is even more expensive. It is also necessary that these cells undergo tests to ensure that they have not mutated or changed in any detrimental way through the reprogramming process. It is a cool idea that everyone could have their own iPS cell line that could be used to make a personalized therapy product for themselves, but in practice this is very time consuming and expensive to do it on a per-person basis. In embryonic stem cell therapies, the generation of the cells has already been performed in the proper ways, and the expensive tests can be performed on a single stem cell line, rather than a different line for every individual.
It is possible that one day iPSCs may prove to be equivalent to embryonic stem cells (ESCs) and could be used in the same way we use ESCs now. However, because iPSCs are a very new discovery (2006), it is still to be determined iPS cells are are equivalent to embryonic stem cells in all ways. Scientists are working hard on understanding the differences that may exist between embryonic stem cells and iPS cells, and we still have yet to determine which cell type will be the most useful for regenerative medicine.