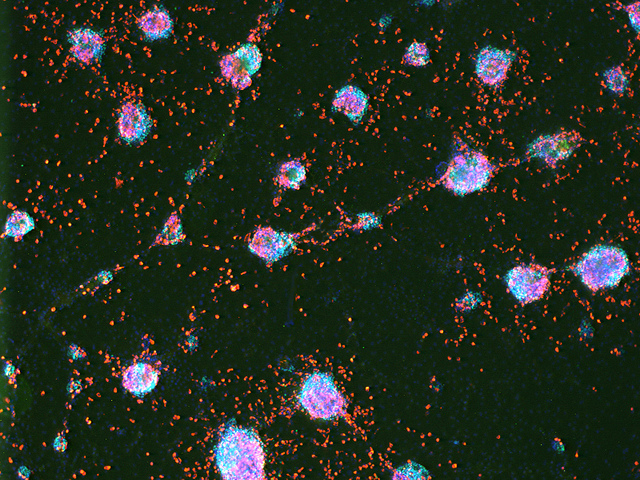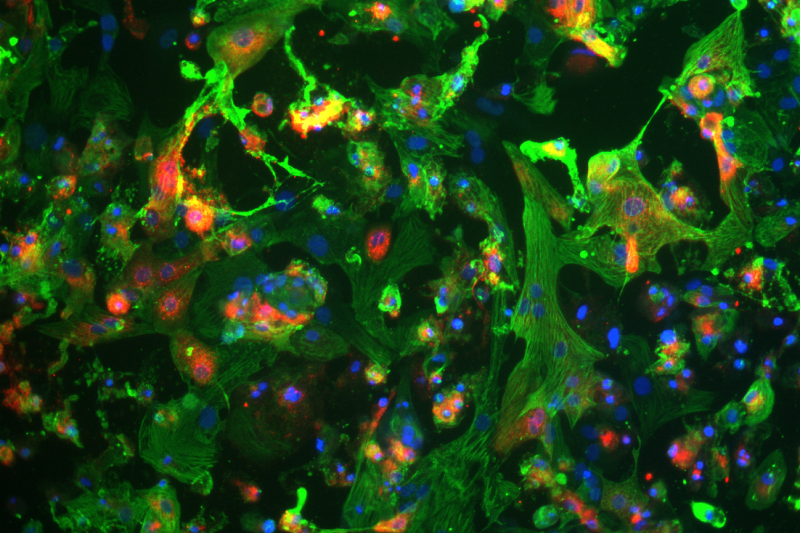
Human induced pluripotent stem cell-derived cardiomyocytes (heart cells) shown in green and blue, are infected by the novel coronavirus SARS-CoV-2 (red). Image Courtesy of UCLA Broad Stem Cell Center
There is still a lot that we don’t understand about SARS-CoV-2 (COVID-19), the new coronavirus that has caused a worldwide pandemic. Some patients that contract the virus experiences heart problems, but the reasons are not entirely clear. Pre-existing heart conditions or inflammation and oxygen deprivation that result from COVID-19 have all been implicated but more evidence needs to be collected.
To evaluate this, researchers at the UCLA Broad Stem Cell Research Center used human induced pluripotent stem cells (iPSCs), a kind of stem cell that can become any kind of cell in the body and is usually made from skin cells. The iPSCS were converted into heart cells and infected with COVID-19 in order to study the effects of the virus.
The results of this study showed that the iPSC-derived heart cells are susceptible to COVID-19 infection and that the virus can quickly divide inside the heart cells. Furthermore, the infected heart cells showed changes in their ability to beat 72 hours after infection.
In a press release Dr. Clive Svendsen, one of the authors involved in this study, elaborated on the results.
“This viral pandemic is predominately defined by respiratory symptoms, but there are also cardiac complications, including arrhythmias, heart failure and viral myocarditis. While this could be the result of massive inflammation in response to the virus, our data suggest that the heart could also be directly affected by the virus in COVID-19.”
Although this study does not perfectly replicate the conditions inside the human body, the iPSC heart cells may also help identify and screen new potential drugs that could alleviate viral infection of the heart.
The research team has already found that treatment with an antibody called ACE2 was able to decrease viral replication on the iPSC heart cells.
In the same press release Dr. Arun Sharma, another author involved in the study, had this to say about the ACE2 antibody.
“By blocking the ACE2 protein with an antibody, the virus is not as easily able to bind to the ACE2 protein, and thus cannot easily enter the cell. This not only helps us understand the mechanisms of how this virus functions, but also suggests therapeutic approaches that could be used as a potential treatment for SARS-CoV-2 infection.”
The full results of this study were published in Cell Reports Medicine.