Three-year-old Ava was constantly sick. Her gums were inflamed, and every time she got a scraped knee, it turned into a dangerous infection.
Her parents, Alicia and Jon Langenhop, were months pregnant with their third child when they learned that Ava’s constellation of symptoms added up to an extremely rare, inherited disorder of the white blood cells, called leukocyte adhesion deficiency-1. Although antibiotics and antivirals could prolong her life, the disease was considered fatal, usually before kindergarten.
Ava’s primary hope, doctors told the Langenhops, was a bone marrow transplant from someone who was a good match, probably a brother or a sister.
Two-year-old Olivia had inherited the same disease as her big sister. She had been hospitalized with infections, too.
The baby in Alicia’s belly would be the girls’ best hope. Since both parents were carriers of the rare genetic mutation, the new baby, a boy, had a 25% chance of inheriting it, too.
Alicia was still in the hospital last October when they found out baby Landon had the mutation. Around the same time, the couple learned of a research trial in California.
Doctors would take each child’s blood cells, fix the mutation and return them. It should be a permanent fix, with less risk than a bone marrow transplant because the healthy cells would be their own, so their bodies wouldn’t reject them as foreign.
The approach had been tried in only one child, though.
This is the type of research reaching patients nearly two decades after President George W. Bush banned federal funding of stem cell research and 16 years after California residents approved a tax increase on themselves to support research.
Proposition 14 on Tuesday’s ballot asks whether Californians want to continue this work, providing $5.5 billion for stem cell research over the next three decades.
In the early 2000s, stem cell research was controversial because it often required the destruction of human embryos. Though embryonic stem cells remain essential for some therapies, in cases such as the Langenhops’, treatment focuses on manipulating a person’s own cells.
Stem cell science has made tremendous progress, but as in most new fields, the pace remains painstakingly slow. Every treatment has to be the subject of years of trial-and-error research, and many scientific hurdles linger.
Stem cells have been used to treat rare diseases, such as severe combined immunodeficiency, also known as “bubble boy disease,” and they are being tested in more common conditions such as Parkinson’s disease, macular degeneration, Type 1 diabetes and even heart disease.
“Even if a subset of stuff in the pipeline goes all the way, it will change the world for patients who currently don’t have other good options,” said Sean Morrison, a stem cell biologist in Dallas.
“It’s a pivotal time in the field,” said Dr. Deepak Srivastava, president of the Gladstone Institutes, a nonprofit research organization based in San Francisco. “We can feel that we’re at an inflection point, where after years of discovery and creating a foundation of knowledge, we’re finally at a point where a number of approaches are reaching clinical trials.”
Watch out for sham treatments
Stem cell therapies haven’t advanced as far as some clinics offering expensive treatments claim.
Getting stem cells injected into your knee, for example, hasn’t been scientifically proven safe or effective – but some clinics charge thousands of dollars for the procedure.
“There are many clinics throughout the world, including in the United States, that continue to market unproven stem cell therapies,” said Timothy Caulfield, a professor of law and public health at the University of Alberta in Canada. “They leverage the excitement that has surrounded this area to push products that aren’t supported by good science. Indeed, there still aren’t many stem cell therapies that are clearly ready for broad clinical application.”
One way to distinguish the good science from the scams, Morrison said, is to look at what’s promised. Anyone who offers to treat different ailments with the same “multipurpose” cells is selling snake oil, he said.
There are a wide variety of stem cells – embryonic stem cells, induced pluripotent stem cells, somatic cells, etc, he said – and it’s challenging to figure out which to use against which disease.
“Every disease is a different set of challenges, and we spend years trying to develop therapies that are safe and effective,” said Morrison, who chairs the public policy committee of the International Society for Stem Cell Research, a scientific organization. “When a company comes out making claims about a one-size-fits-all therapy that can treat everything, that’s a sure sign that they’re just trying to take your money.”
Stem cells in California
Several researchers interviewed by USA TODAY said state funding helped put California at the forefront of global stem cell research.
George Daley, a stem cell biologist who is dean of Harvard Medical School, said he’s envious of the California researchers who have access to this pot of money.
“California has always been a very exciting place to pursue science, but prior to (the taxpayer funding), it wasn’t exactly the place that was the first on the tip of your tongue as a powerhouse community for stem cell science,” he said. “But there’s no way that today it wouldn’t be listed in the top three.”
Daley, a global leader in the field, said he thinks the funding spurred enthusiasm for stem cell research more broadly. “The entire excitement around the field of stem cell biology is part of the reason you’re seeing cures in cancer and impending cures in devastating diseases like sickle cell anemia,” he said.
Although stem cell therapy hasn’t gotten anyone out of a wheelchair yet, he said important research continues that may eventually transform paralyzed patients’ lives. “If it’s taken us longer than people anticipated, that’s just the pace of science,” he said.
Research begun in the Harvard lab of Doug Melton may soon revolutionize treatment of Type 1 diabetes, he said, liberating patients from needing to inject themselves daily with insulin.
Srivastava, a cardiologist, admitted that the field, backed by federal funding, spent more than a decade chasing cardiac stem cell treatments that never succeeded, possibly because they weren’t stem cells at all.
Now, his lab and others have modified true stem cells into beating heart cells, he said, which should one day be able to restore tissue damaged by a heart attack.
The big bottleneck in the field, Srivastava said, is getting cells to fully mature in a dish. Scientists can turn stem cells into immature cells of many different types – neurons, heart cells, retinal cells – but they get stuck in this fetal-like state.
Beating heart cells derived from stem cells can create rhythm disturbances because they’re electrically different from normal, mature cells, he said.
“It would be beneficial to have a cell that could function more like a cell after birth,” Srivastava said.
Turning stem cells into cures
Donald Kohn, the Langenhops’ doctor at the University of California-Los Angeles, has been involved in stem cell research since 1985.
“I’ve seen it go from a dream, a vision, to now just various degrees of how it’s working,” said Kohn, also a member of the UCLA Broad Stem Cell Research Center. About a dozen blood diseases such as LAD-1 have shown “very good clinical responses” to the type of treatment the Langenhop children received.
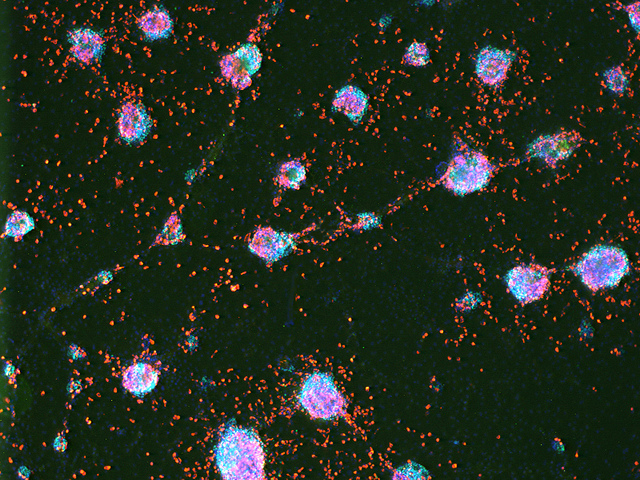
The children are missing a protein in their white blood cells that would allow the cells to reach a cut or damaged tissue. The children can’t clear infections, and suffer from inflammation and other immune-related problems.
Kohn’s study of kids with LAD-1 mutations will eventually include nine patients. Depending on the results, the company sponsoring the trial, Rocket Pharmaceutics of New York, will ask the U.S. Food and Drug Administration for a license to sell the therapy.
He said he’s been blown away by how well the Langenhops have dealt with the trials and tribulations of the past year.
“I just think they’re heroic, what these parents are doing,” Kohn said.
Dealing with the unimaginable
At first, the Langenhops asked themselves how a disease that strikes fewer than 1 in a million children could have struck them three times.
But now, more than a year after Ava’s diagnosis and six months after temporarily moving to California for the treatments, Alicia and Jon just want to bring three healthy kids home to Canton, Ohio.
They flew to California for the first time last December so doctors could collect bone marrow cells from Ava. They’d planned to come back in February for the treatment, but not enough cells had been repaired, so the February trip was just a repeat of December.
By the time they were ready to come back for her therapy in late April, the pandemic had struck. The airplane was nice and empty.
Ava got chemotherapy twice a day for five days to kill off her faulty white blood cells. After a day of rest, she was given back her own blood stem cells, gene-edited to remove her damaging LAD-1 mutation.
Her one complaint: the therapy smelled like creamed corn and made her gag.
She recovered quickly, and after about a month in the hospital, enough white blood cells had grown back for her to safely return to the family’s rental apartment, just off the UCLA campus, where her mom has turned the living room into a classroom for the girls.
Although she lost all her hair from chemo, it’s slowly growing back, and she’s very proud of her cropped hairstyle, Alicia said. She picks out a bow every day to match her outfit.
At Ava’s three-month checkup this summer, doctors found her bone marrow was producing healthy white blood cells. Her LAD-1 is considered eliand she’ll never need another treatment.
“She’ll probably be healthy forever,” Kohn said.
Landon, age 1, completed his treatment about a month ago and was allowed out of the hospital last week. He’s bald, but his blue eyes still sparkle, and as he waved through the camera on a recent Zoom call, it’s hard to imagine a cuter, healthier-looking baby.
Although originally slated for treatment before her brother, Olivia, 3, ended up last, because, as with her sister, the processing of her cells didn’t work well the first time. She went in the hospital Sunday and starts her chemo Monday night. She is scheduled to receive the corrected cells next week.
Olivia was excited to start her therapy, to be “part of the club” with her sister and brother, Alicia said. “She can’t wait to turn bald.”
The cost of all three childrens’ treatments and the rental apartment and plane fare are being picked up by Rocket Pharmaceuticals. That’s the upside of volunteering for clinical trials: the treatment is paid for by the sponsor.
Jon was a bank branch manager before the pandemic, and now works remotely for the same bank, reviewing loan applications. “It gives me the chance to be at the hospital with whichever child is in the hospital at that time,” Jon said, chuckling.
Alicia, a former teacher and day care center assistant manager, has been homeschooling the kids since the start of the pandemic.
Their doctor hopes to have the family back in Canton for Christmas or at least New Year’s. The weather won’t be as nice as in Southern California, but they’ll be home, surrounded by their supportive family and friends. And Jon and Alicia won’t have to worry anymore about every scrape and sniffle.
They don’t focus much on the details of how the science works. They’re just happy it has.
“We feel so fortunate to be living in a time when this is possible,” Alicia said.
If they had been in this situation even a few years ago, the treatment wouldn’t have existed, Jon said. If they had found out about Ava’s mutation when she was younger, they wouldn’t have had two more children.
“It’s kind of crazy how it’s all worked out for us,” he said.
The strength of their kids has given them strength. “They just go with the flow. It’s kind of incredible how resilient they are and can just bounce back from these hospitalizations,” Jon said.
“Like nothing ever happened,” Alicia added.
The three children will probably have few if any memories of their disease and treatment. For Jon and Alicia, however, this year is seared into their memory.
“It’ll take us a while to realize they don’t have this anymore,” Jon said.
Karen Weintraub can be reached at [email protected].
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.