I had planned that our next story would be about ALS, Lou Gehrig’s disease. But I must hold up on that for a week or so—I called some people doing amazing work on it, and I want to interview them first.
Instead, let’s take a trip to the Valley of Death.
In the world of biomedicine, there is a place you will not find on any map. It has no physical existence—but it is, all too often, where new medicines go to die.
To understand the “Valley”, ask yourself a question: why do new drugs and therapies cost so much?
Part of the reason is sheer greed, no question about it. The love of profits motivates some people stronger than sex and doughnuts. Martin Shrekeli raised the price of one pill from $13.50 to seven hundred fifty dollars— for the same one pill.
Such people seem to have an endless lust for money, no matter who gets hurt.
But there is another and far more legitimate reason for high drug costs, and that is the astonishing expense of endless tests, both for safety and “efficacy” (does it work?) required by the FDA.
How much does it cost to bring one new drug or therapy through the “valley of death” of FDA testing, both animal and human? Brace yourself:
Costs range from $2.6 to $3.9 billion dollars to take one drug through all the tests.
If a company can’t raise the money, their new drug or therapy never goes to market, never reaches a patient—and the valley of death blocks cure again.
Don’t get me wrong, I respect the FDA; we need the good work they do. Nobody wants a medicine that does nothing, or that makes people worse. Did you hear about the three ladies who recently paid to have adult stem cells made from their own fat tissues—and it made them blind?
But we need the research to go forward at all reasonable speed, and that is just not happening.
One stem cell therapy (Hans Keirstead’s ground-breaking paralysis work, with early research paid for by the Roman Reed Spinal Cord Research Act of 1999) has been in testing for almost two decades. (With clinical trials partly funded by CIRM, it is proving its value; having recently restored hand function to 6 out of 6 newly paralyzed patients.)
We need to find a better way.
And maybe, just maybe, the California stem cell program can provide that way: to not just speed up testing and lower the costs for stem cell therapies, but perhaps for all new medicines as well.
Consider: what if, instead of having to make up new test after test after test—each original and therefore expensive—we had an FDA-approved testing center, where scientists and patients could go and get the testing done: all set up, ready to go, like plug and play for a computer program?
That is the idea behind CIRM’s Alpha Stem Cell Clinics.
The California stem cell research started off with three sites—San Diego, a combined site of the University of California at Los Angeles and UC Irvine, and the City of Hope. There is also a stem cell center* to coordinate the storage of new information, and assist patients and physicians with questions.
Yesterday, in an all-day meeting of the program’s board of directors (Independent Citizens Oversight Committee, or ICOC), a decision was reached to add two more: one at the University of California at Davis, and the other of University of California at San Francisco.
Each “Alpha Site” reaches a different patient community, hopefully allowing people from all across the state to have access to stem cell clinical trials closer to them. UCSF, for instance, will reach Northern California and the Bay Area.
Will the Alpha Stem Cell Network accelerate progress toward curing chronic diseases and disabilities?
Follow CIRM and find out. I strongly suggest subscribing to their outstanding weblog.
https://www.cirm.ca.gov/about-cirm/e-newsletters
*The Alpha Stem Cell Network will be coordinated by a Stem Cell Center in San Diego. For more information, email them at: [email protected].
This post originally appeared on HuffPost.
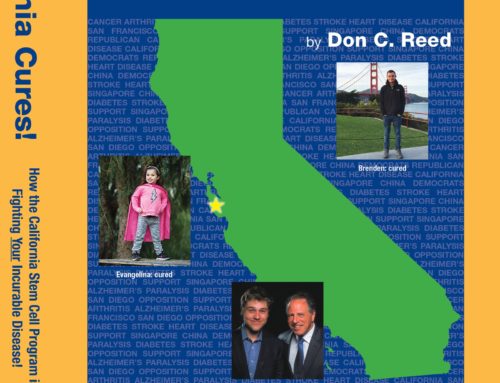
Don C. Reed is Vice President of Public Policy for Americans for Cures, and he is the author of the forthcoming book, CALIFORNIA CURES: How California is Challenging Chronic Disease: How We Are Beginning to Win—and Why We Must Do It Again! You can learn more here.