“You ought to get a computer!” said my cousin Tommy Snyder, a couple of decades ago, “It would help you write your books!”
“Sure,” I snapped, ”Next time I get an extra $5,000 (computers cost a lot back then) I will just dash right out and get one!”
Months passed, and I forgot about the seemingly casual remark.
And then suddenly, there was my cousin, knocking on the door. He had a big beaming smile on his face and a box in his arms: a Macintosh computer.
Tommy had organized my family to raise the money. His father, my Uncle Ben, was one of the primary funders of this greatest material gift of my life.
I wish I had a happy ending for my Uncle’s story.
But Ben Snyder developed End Stage Renal Failure: his kidneys ceased to function. No longer would they filter his blood, transferring the poisons of cellular waste into the urine, to pass safely from the body; instead the toxins accumulated.
He had to endure hemodialysis: blood washing. Three times a week he went to the hospital. Two needles stabbed into his arm, and a massive amount of blood (60–70%) was withdrawn, passed through a filter, and then replaced. The procedure took three hours.
It kept him alive for several years, but then he died: a good man, taken too young.
Today, kidney disease affects a staggering number of people: thirty million in America alone. Many more may have it, but not yet diagnosed.
https://www.kidney.org/news/one-seven-american-adults-estimated-to-have-chronic-kidney-disease
And the end stage condition which took my Uncle’s life?
“Over 650,000 Americans suffer… (the) life-threatening condition caused by the loss of kidney function.”
— Kevin McCormack, CIRM Press Release, January 18, 2018.
So, what’s to be done?
CIRM (the California Institute for Regenerative Medicine, our hard-won state stem cell program) is tackling the kidney disease from several directions.
Andy McMahon, a developmental geneticist, is studying the natural development of the kidney. By studying its biology, he hopes to learn how a healthy kidney repairs itself, especially since they do not appear to have stem cells of their own…
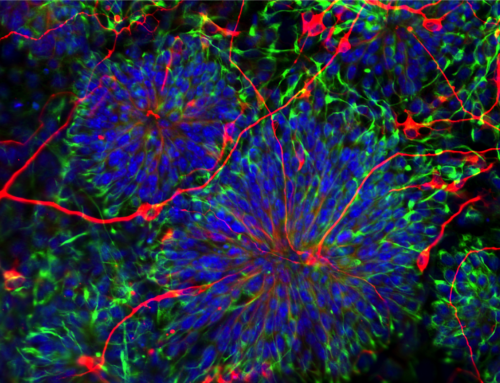
Have you heard of “organoids”? These man-made mini-organs may provide a great avenue for drug testing — instead of trying a new therapy on a person, we can try it on a “sick” glob of tissue, with no risk to people. This would speed up the safety and efficacy trials, and greatly lower the costs of new drugs.
Down the road, some feel, organoids may be used as actual replacements for various parts of the body.
But whether for testing (disease in a dish) or replacement, the organoid must be “relevant” (similar to the organ being studied) as Andy said in a recent phone interview.
For instance, a key element of the kidney is the nephron, a microscopic human tube, which helps in the filtering process. Dr. McMahon wants to develop nephrons, (perhaps a million per kidney) and learn how to protect or replace them.
Another approach is transplantation. When a kidney donor can be found, (difficult but possible, best bet is from a relative) the new kidney has to be installed and accepted by the body. To prevent rejection, drugs called immunosuppressants must be used. These can cause very serious difficulties — infections, heart disease, cancer, diabetes, all manner of bad stuff.
However, a CIRM-funded company, Medeor Therapeutics, may have the answer.
Injecting stem cells and immune cells from the donor may make his/her transplant organ “fit in”, and not be rejected.
“Medeor’s stem cell-based therapy aims to prevent transplant rejection, and eliminate the need for immunosuppression…” said CIRM President Maria T. Millan…”If they are successful, this approach could be developed for other organ (transplants) including heart, liver, and lung….”
Still another approach, this one by Humacyte, Inc., will be to use stem cells to make the dialysis process safer: by using a bioengineered vein. Instead of a plastic tube inserted into the arm, with risk of infection, a “bioengineered vein is implanted in the arm and used to carry the patient’s blood to and from their body during dialysis.”
https://www.ncbiotech.org/news/humacyte-gets-10m-boost-clinical-trial
The tube would gradually become part of the patient’s body, as “the patient’s own stem cells …populate this vein”.
Which avenue will help the most and the fastest? Perhaps all, perhaps none — maybe something entirely different. We can only find out through funding science.
But whether replacement or repair, new nephrons or biomedical tubing, it is clear that something major must be done.
Because with one American in seven suffering kidney disease, almost everybody has an Uncle Ben.
Don C. Reed is Vice President of Public Policy for Americans for Cures, and he is the author of the forthcoming book, CALIFORNIA CURES: How California is Challenging Chronic Disease: How We Are Beginning to Win—and Why We Must Do It Again! You can learn more here.