Forty-five years ago, when my daughter Desiree’ was about to be born, I was there in the delivery room, to support Gloria, and to greet our daughter into the world.
I was not entirely sure what to expect. I had seen a medical movie about the birthing process, which struck me as unnecessarily graphic. Gloria said my face went pale in certain parts. She patted my hand and told me everything would be all right.
We were, we hoped, prepared. We had practiced all the LaMaze breathing techniques, night after night.
The delivery? Fantastic. Gloria strained her muscles and shouted like an athlete, like lifting weights in the Olympics. I stood at her head and tried to stay out of the way. Back then, a husband’s presence in the birthing room was not usual, and I had been warned I would be ejected if any problems arose, if I fainted, for example. But Gloria hollered and words came like “crowning!” and “I can see the head!”
Suddenly, the doctor put a baby in my arms: Desiree’ Don Reed, middle-named in pride after me… She smiled, then turned her attention to her fingers, closing them, making a fist, like hmm, what do we have here?
The nurse took her from me, and I felt like growling. But an intern handed me a container of green Jell-o, told me Gloria could eat something now.
But she was too tired to chew. The little green chunks fell out of her mouth.
And then I saw it, the placenta: this limp torn plastic-looking little white bag. There were a few streaks of blood on it, but my emotional reaction was completely the opposite of what I expected. I felt…gratitude. In my mind I actually said “thank you” to it, to the placenta, which had sheltered my daughter inside her mother, protecting her all those long months.
But what if there had been something wrong with the placenta, that interface/connection between mother and unborn child? Hold that thought.
Remember the sword-fighting scene in Shakespeare’s MACBETH? Two warriors, Macbeth and Macduff, are dueling to the death, and Macbeth tells his rival he is protected by magic and cannot be killed “by any man of woman born”.
But Macduff doesn’t care.
“From my mother’s womb, I was untimely ripped”, he says.
“Then lay on, Macduff, and damned be he who first shall cry enough,” shouts the Scottish lord. The swordfight continues, and Macbeth loses his head, literally.
We are not told, but apparently Macduff’s mom gave birth to him prematurely.
And what is the primary cause of premature delivery?
Pre-eclampsia…
“Pre-eclampsia is a pregnancy complication…(which) threatens 5–8% of all pregnancies. It has major effects on blood pressure and kidney function of the mother.
“It is responsible for a significant proportion of maternal deaths and growth-restricted babies…”
I had not considered that. We had gone into the hospital to have a baby, and our thoughts were on the soon-to-be-born child — but Gloria could have been at risk?
And the same condition, pre-eclampsia, could have caused our child to be born prematurely?
“On an average day in California, 149 babies are born prematurely. Many of these babies will require weeks of care in an…intensive care unit… at an average cost…$25,000…compared to $1,500 (for) a baby born at term…”
Dr. Mara Parast, of the University of California at San Diego, is trying to reduce that suffering.
A difficult challenge.
The usual test subjects, rats and mice, do not get the disease the same way.
So how do you test drugs to find out their effects on humans?
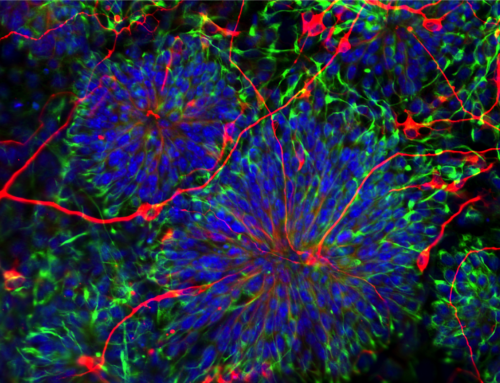
Consider a stem cell angle.
The problem in pre-eclampsia is too few “trophoblasts” a special kind of stem cell that builds and repairs the placenta. There are two kinds of trophoblasts, one to share blood between baby and mom, the other to pass nutrition along.
Want to know two giant words you will probably never use in your life?
Syncitiotrophoblast, and extravillustrophoblast.
One is for making blood, one is for transferring food to the little one.
I remember which is which, by thinking, “eating is a sin” (well at least the way I do it!), so syn-city-o-trophoblast. And the other, well, that is the other!
Dr, Parast has made a stem cell model of the diseased trophoblasts , and another model of healthy ones, to compare the differences, maybe find a way to use the healthy stem cells to combat the sick ones — and also test new medications.
“Parast’s work focuses on the stem cells that give rise to the placenta, …trophoblast stem cells. Her lab has created a human trophoblast stem cell model — a first — that can be used to study stages of placental development. The CIRM grant will fund continuation of this work…to identify potential stem cell based therapies for treating pre-eclampsia without resorting to premature delivery.”
Valuable project, would you agree?
But what if this outstanding young doctor could not get a grant? The average age for first grants from the National Institutes of Health (NIH) nowadays is 44 years. Dr. Parast is far younger than that. Just to meet expenses, she could be forced to work in so many other directions that she would not have time for stem cells?
Bob Klein is the man who began the citizens’ initiative Proposition 71, which became the $3 billion California stem cell program.
I asked him, what did he think were the most important grants?
He said the grants that helped young scientists to survive financially while trying to survive in the stem cell research field.
All across the country, research funds are increasingly difficult to find.
The primary source of medical research funding, the National Institutes of Health (NIH) was scheduled for a 20% cut in the first Trump budget. 20%! The NIH has been flatlined for many years; it needs a massive increase, not a cut.
Many worthwhile projects are just not getting done.
But the California Institute for Regenerative Medicine is helping where it can, establishing 4 separate grants with that purpose:
New Faculty grants I (given to 22 investigators) and II (23 recipients), plus the Physician Scientist Translational Research Awards (15) — and the Medical College Repayment Award, which went to 5. –Dr. Pat Olson, chief scientist, CIRM, personal communication.
That is 65 scientists who might otherwise been unable to fund their research, maybe not even have been able to stay in the field. Instead, they are working.
Dr. Arlene Chiu, former Chief Scientific Officer, remembers:
“These grants are designed to encourage newly independent investigators to pursue bold and innovative studies across the full range of stem cell types…providing successful applicants salary and research funding for up to five years, ensuring that they have stable, secure financial support as they begin their … scientific careers.”
Providing a base of stability for brilliant new scientists is just one of the many reasons the California stem cell program was made.
And why it must go on.
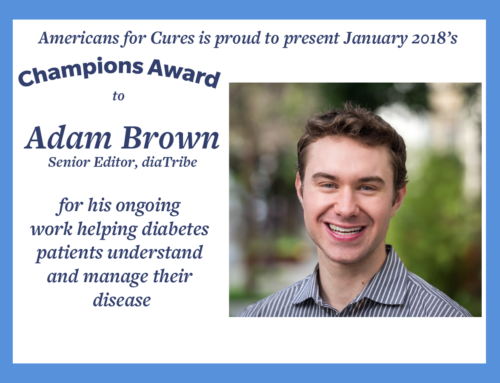
Don C. Reed is Vice President of Public Policy for Americans for Cures, and he is the author of the forthcoming book, CALIFORNIA CURES: How California is Challenging Chronic Disease: How We Are Beginning to Win—and Why We Must Do It Again! You can learn more here.